Version 4.1.8
|
|
OneView Physician Quality Release Notes
What's New in OneView Physician Quality 4.1.8
Release Date: Tuesday, July 25, 2017
Acmeware is pleased to announce that our One View Physician Quality package version 4.1.8 is available for general release. Version 4.1.8 adds new functionality and support for eReporting for the 2017 reporting period electronic clinical quality measures (eCQM) including the latest 2016 eCQM specifications from CMS.
OneView 4.1.8 includes 2017 Performance Period eCQM specifications (as of January 2017) updates to nomenclature mapping codes, logic corrections, updated value sets from the NLM Value Set Authority Center and updated clinical best practices guidance from MEDITECH. We have included support for 2017 MACRA/Merit-Based Payment Incentive System (MIPS) program, Comprehensive Primary Care (CPC) Plus eCQM, and Modified Stage 2 program requirements for Eligible Professionals Attesting to their State’s Medicaid EHR Incentive Program.
OneView 4.1.18 now includes built-in support for MEDITECH’s Oncology application including MAGIC, CS, and MAT61.
Here's a summary of what's new in this update:
New Quality Programs: OneView Physician Quality (PQ) continues to support Medicaid Meaningful Use CQM and Objective Measure reporting and attestation. OneView Medicaid Objective Measure updates were made to conform to the Modified Stage 2 EP Objective specifications published by CMS in the Electronic Health Record Incentive Program-Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 published 10/16/2015, and the CMS OPPS Final Rule published 11/14/2016.
In addition, OneView PQ now supports the Merit-Based Payment Incentive System (MIPS) program including Quality, Advancing Care Information (ACI), and Improvement Activities (IA) reporting and submission. New workflow associated with the 2017 reporting period requirements will need to be reviewed and incorporated to ensure that these items are accurately configured for this new release.
Lastly, OneView PQ now supports Comprehensive Primary Care Plus (CPC+) eCQM Reporting.
Submission Wizard: The ability to create electronic submission for 2017 has been disabled until the next release. New workflow associated with the 2017 reporting period requirements will need to be reviewed and incorporated to ensure that these items are accurately configured for this new release. As a quality reporting submission vendor, Acmeware has a fiduciary responsibility with clinical quality reporting to CMS. Due to Acmeware standard and these significant changes, we have disabled the lock functionality in this release and it will be reinstated in the next release.
Customer Support Portal: You can create new OneView report requests and other service issues using the Customer Support Portal, as well as see the status and all relevant communication about your support tickets. While use of the portal is optional, as we remain available via telephone and email, we've found that the new system has helped us improve our communication with clients, as well as more easily organize their report requests, issues, and questions.
For more information about the Customer Support Portal system and new user registration use the following link: https://support.acmeware.com/User/Register
New Features/Enhancements:
Merit-Based Payment Incentive System (MIPS):
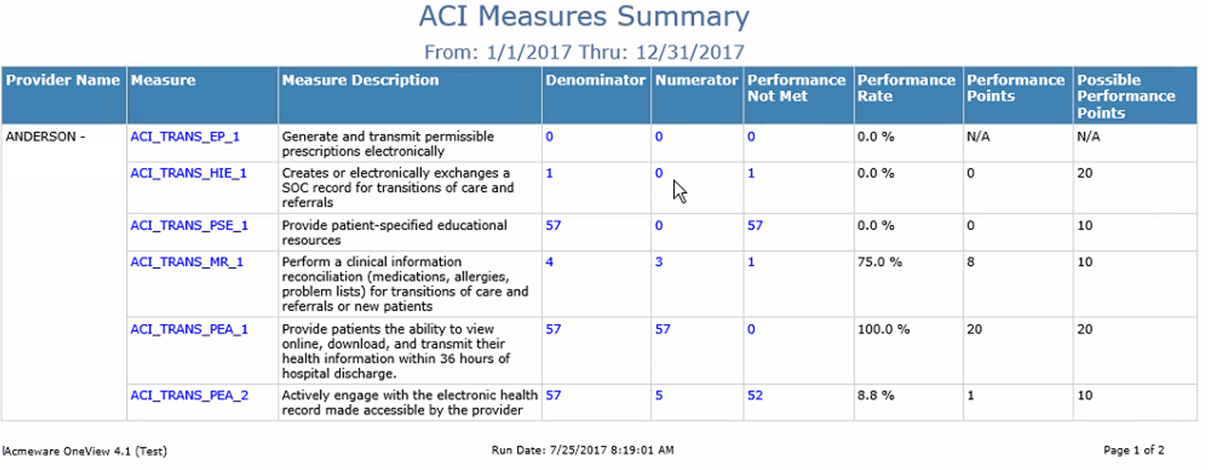
- Advancing Care Information (ACI) category reporting support for all measures
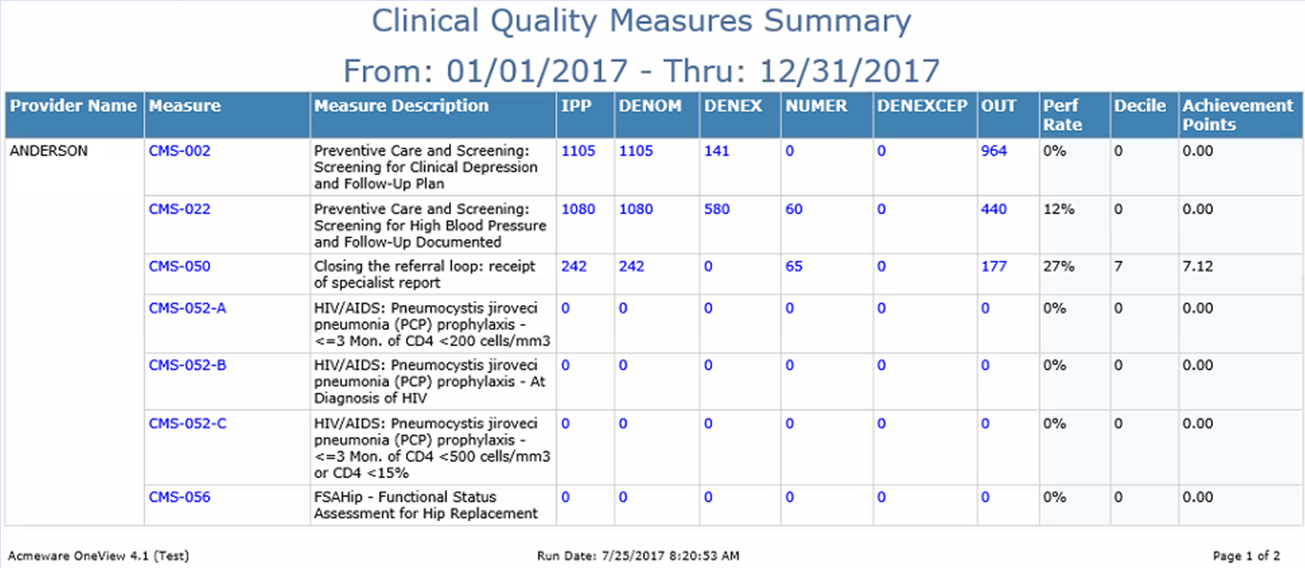
- Quality category reporting support for all measures
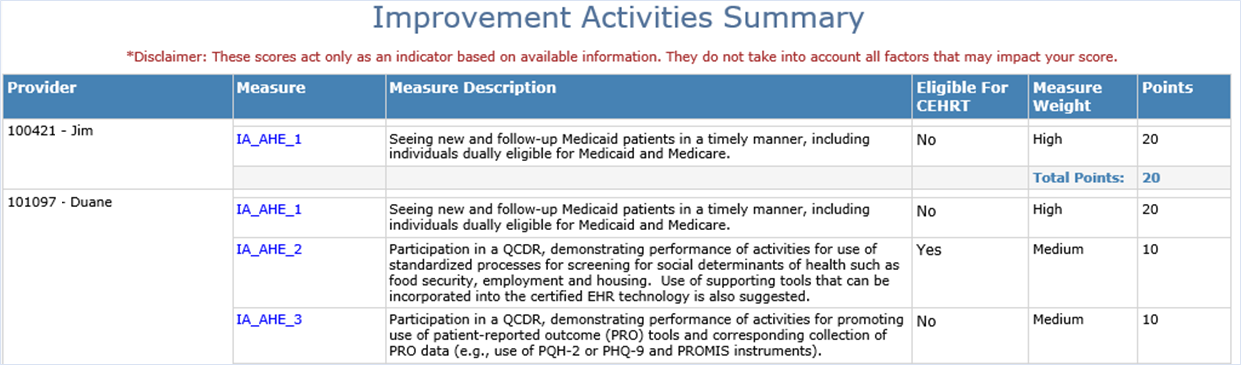
- Improvement Activities (IA) support for tracking measure selection
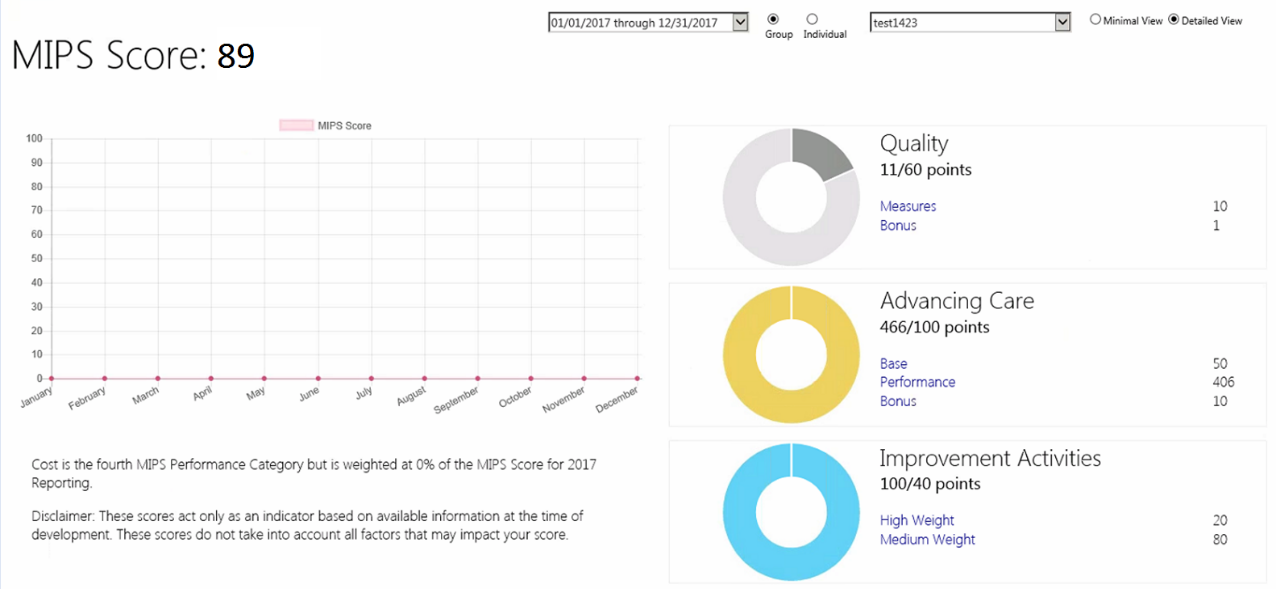
- MIPS Dashboards for advanced category scoring
Changes to the 2017 Stage 2 Medicaid Objective Measures:
- All Measures:
- Support for Medicaid.
- Updates to reports based on new timing requirements released in CMS FAQ # 8231.
- Implement Patient Portal 2.0 when available.
- Patient Electronic Access:
- Support for MEDITECH Portal 2.x
- CPOE:
- Updated logic so order date must be a valid date.
- Updated logic to insure CPOE measures are taken during reporting period.
- For 2017 Stage 2 Objectives, the CPOE objective is ONLY required for eligible hospitals and critical access hospitals who attest Medicaid only.
- Electronic Prescribing:
- Updated reports to including all but Pending orders so it matches MEDITECH updates.
- Updated reports to exclude over the counter medications, durable medical equipment and controlled meds unless schedule is defined by customer
Changes in the 2017 Reporting Period Specifications (as of January 2017):
Review changes noted in the update specifications and in the MEDITECH best practice text to make sure your facility’s set-up requirements.
- Adjusted OneView populate logic to support QRDA category 1 changes and enhancements.
Reporting Updates:
- Advancing Care Information
- Improvement Activities Summary
- Clinical Quality Measures Summary
- MIPS Dashboard

- Enhancements have been made to the detailed drilldown reports to display QDM Variables at the bottom of the report aligning the report more closely with the CMS specifications. In addition, we removed the ability to click on the variable link to popup a new window with the variable description.
Manage Dictionaries:
- Added a new dictionary called ‘Manage Individual Providers’ and ‘Manage Provider Groups ‘to allow users the ability to associate providers, category and measures to a submission program. The Manage Individual Providers and Manage Group Providers now includes Objective Measures and Improvement Activities in the dictionary setup.
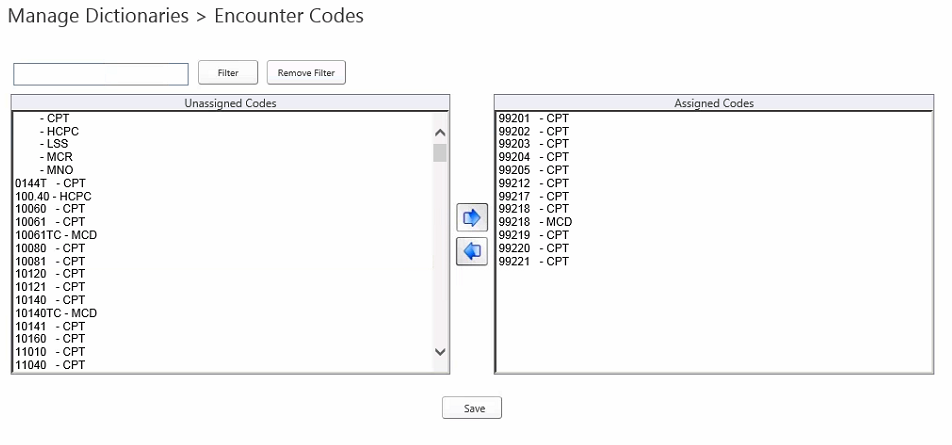
- Added a new dictionary called ‘Encounter Codes’ to allow users to indicate which B/AR alternate codes (SNOMED, CPT, HPCS) will count for the Denominator in OneView Advancing Care Information (ACI) Measures. For ACI reporting, the OneView adds a patient to the Denominator if the patient was seen by the MIPS eligible clinician during the performance period. For patient-based measures, the patient can only be counted once toward the measure. Please review each specification for the Denominator requirement. Please be sure to also indicate which B/AR alternate codes (SNOMED, CPT, HPCS) will count for the Denominator in OneView.
- OneView determines whether the patient had an applicable visit with the eligible clinician (EC) by checking the procedures posted to the patient's patient account. OneView is specifically looking to the Alternate Code defined in the Encounter Codes manage dictionary, not the Procedure Code. Please note the specific Alternate Code will also need to be selected in Managed Dictionaries under Encounter Codes.
OneView Platform:
Enhancements have been made to make it easier for clients moving to a newer MEDITECH platform.

