Version 5.0.1
|
|
OneView Physician Quality Release Notes
What's New in OneView Physician Quality 5.0.1
Release Date: Monday, July 2, 2018
Acmeware is pleased to announce that our OneView Physician Quality package version 5.0.1 is available for general release. Version 5.0.1 adds new functionality and support for eReporting for the 2018 reporting period electronic clinical quality measures (eCQMs) including the latest eCQM specifications from CMS.
OneView 5.0.1 includes 2018 Performance Period eCQM specifications (as of January 2018) updates to nomenclature mapping codes, logic corrections, updated value sets from the NLM Value Set Authority Center and updated clinical best practices guidance from MEDITECH. OneView 5.0.1 includes built-in support for ALL MEDITECH platforms including MAGIC, CS, 6.0, and Expanse.
Here's a summary of what's new in this update:
2015 Edition Certification: Acmeware has completed and passed all certification testing for OneView 5.0 2015 Edition Certification for the Physician Quality Package. We should receive an official certification letter early July and the OneView product should be available on the CHPL website.
Below is a list of all certification criteria completed:
170.315(c)(1) Clinical quality measures (CQMs) - record and export
170.315(c)(2) Clinical quality measures (CQMs) - import and calculate
170.315(c)(3) Clinical quality measures (CQMs) - report
170.315(c)(4) Clinical quality measures (CQMs) - filter
170.315(d)(1) Authentication, access control, authorization
170.315(d)(2) Auditable events and tamper-resistance
170.315(d)(3) Audit report(s)
170.315(d)(5) Automatic access time-out
170.315(d)(6) Emergency access
170.315(d)(7) End-user device encryption
170.315(d)(8) Integrity
170.315 (d)(9) Trusted connection
170.315(g)(2) Automated measure calculation
170.315(g)(4) Quality management system
170.315(g)(5) Accessibility-centered design
Quality Programs: OneView Physician Quality (PQ) continues to support Medicaid Meaningful Use CQM and Objective Measure reporting and attestation. OneView Medicaid Objective Measure updates were made to conform to the Modified Stage 2 EP Objective specifications published by CMS in the Electronic Health Record Incentive Program-Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 published 10/16/2015, the CMS OPPS Final Rule published 11/14/2016 and the CMS IPPS Final Rule published 10/04/2017.
In addition, OneView PQ supports the Merit-Based Payment Incentive System (MIPS) program including Quality, Advancing Care Information (ACI), and Improvement Activities (IA) reporting and submission. Workflows associated with the 2018 reporting period requirements will need to be reviewed and incorporated to ensure that these items are accurately configured for this new release.
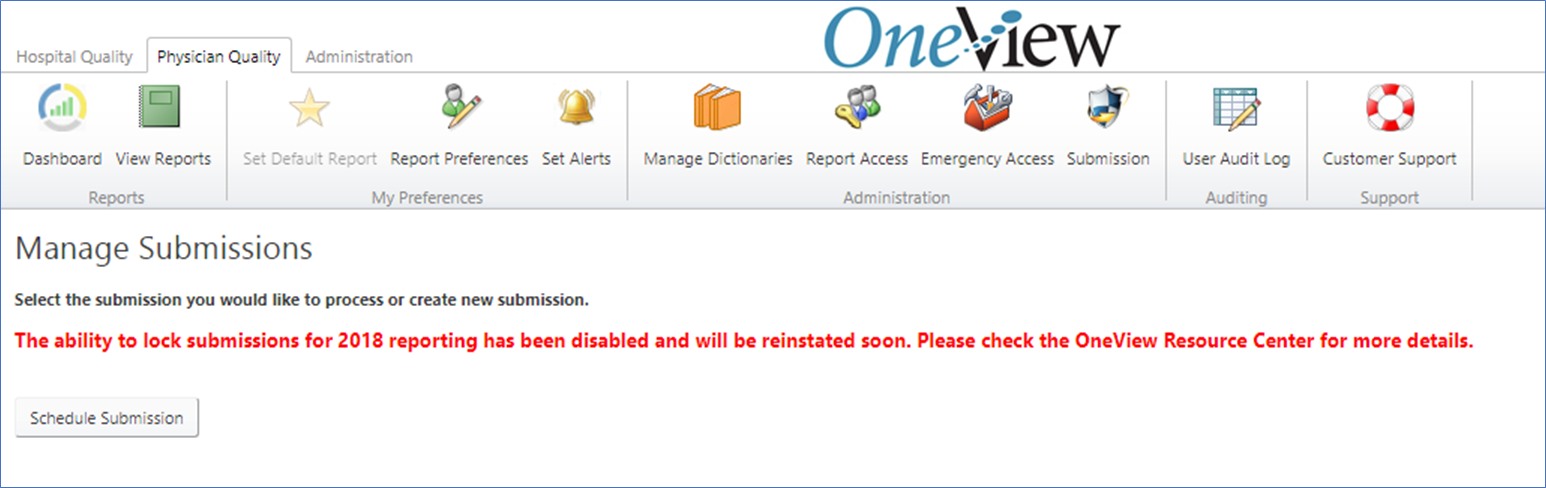
Submission Wizard: The ability to create electronic submission for 2018 has been disabled and will be available in an upcoming release. Workflows associated with the 2018 reporting period requirements will need to be reviewed and OneView output data validated to ensure that these items are accurately configured for this new release. As a quality reporting submission vendor, Acmeware has a fiduciary responsibility with clinical quality reporting to CMS. Due to Acmeware standards and these significant changes, we have disabled the lock functionality in this release but it will be reinstated, as appropriate.
Validation Reporting: Please review our help guide on Validation Reports and Mapping Reports. The help guide will highlight the tools OneView has available to assist in your measure validation process.
- OneView PQ Help Guide - Validation Reports - https://support.acmeware.com/KB/View/3175-oneview-pq-help-guide--validation-reports
- OneView PQ Help Guide - Mapping Reports - https://support.acmeware.com/KB/View/3176-oneview-pq-help-guide--mapping-reports
Known Issues:
- ACI/OM Reports Summary report runs slow when ALL Providers and ALL Measures are selected; it could take up to a couple minutes to complete. If specific providers and measures are selected, the report runs faster.
- The MIPS Dashboard is not calculating the ACI category score correctly.
New Features and Enhancements: (for all platforms unless specified)
Web Application:
- To comply with CMS’s final rule for 2018, the Quality category contributes to 50% of total MIPS score which decreased from 60% in 2017. OneView has been updated to adjust the MIPS dashboard to report the new percentage.
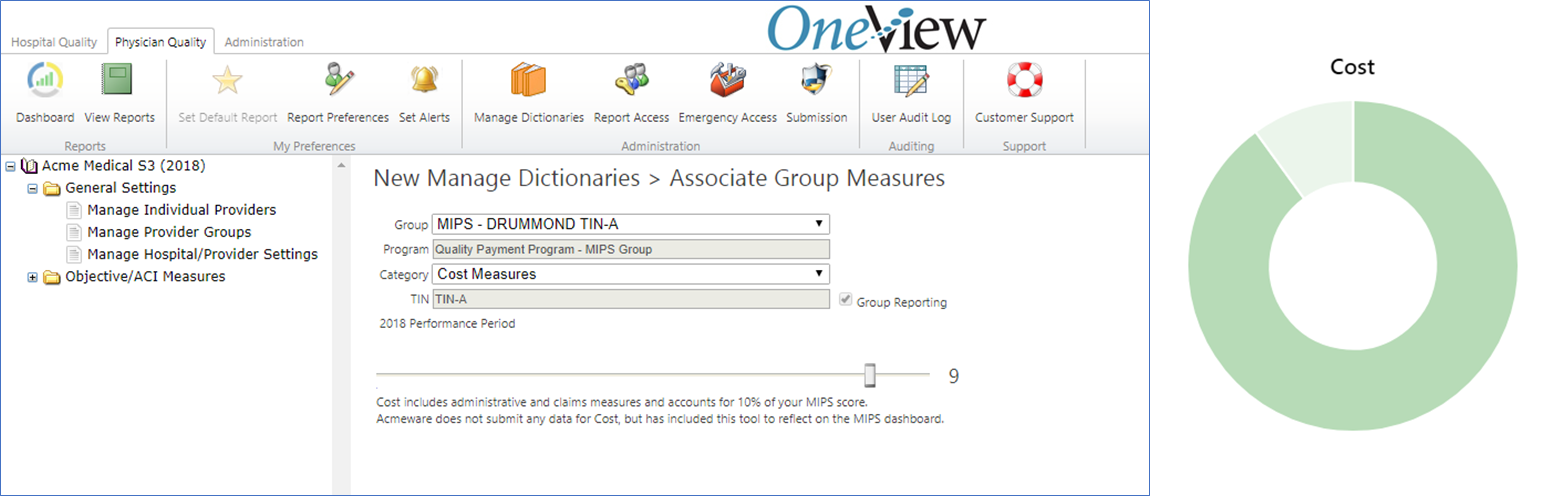
- We have added a new category called Cost to the Manage Dictionaries to allow users to set the reporting percentage of the cost category. The cost category will be managed using a slider from 0 to 10 to allow users to define the Cost score. The Cost score selected will be reflected on the MIPS dashboard.
- As part of the ribbon package update, the hospital settings will no longer be available from the ribbon. Users will be able to access the form from the Manage Dictionaries under the General Settings folder called Manage Hospital Settings.
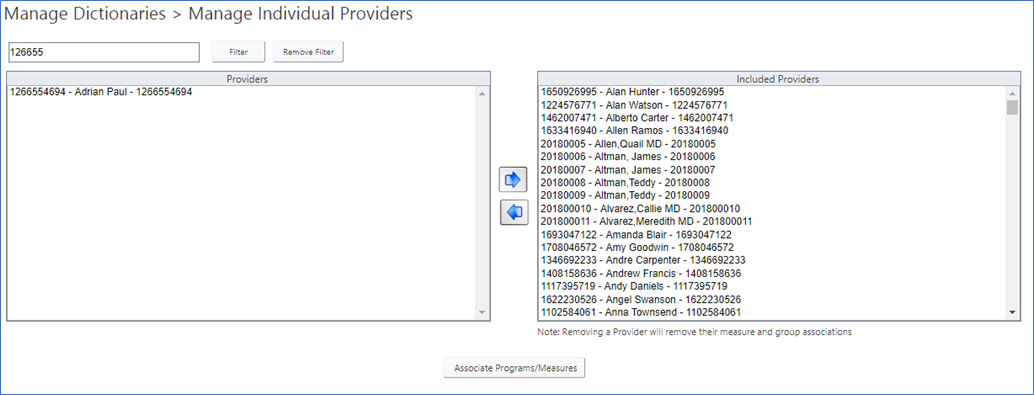
- Updated Manage Individual Providers and Group Providers to add filtering by National Provider Identification (NPI).
Manage Dictionary:
- Created a new item in Manage dictionaries called Location Exclusion to allow for exclusion of locations (ex. psych and rehab units). If you have questions regarding using this dicationary, review the CMS FAQ 10591 we have posted to our Knowledge Base.
Reports:
- Improved runtime performance for ACI and OM reports.
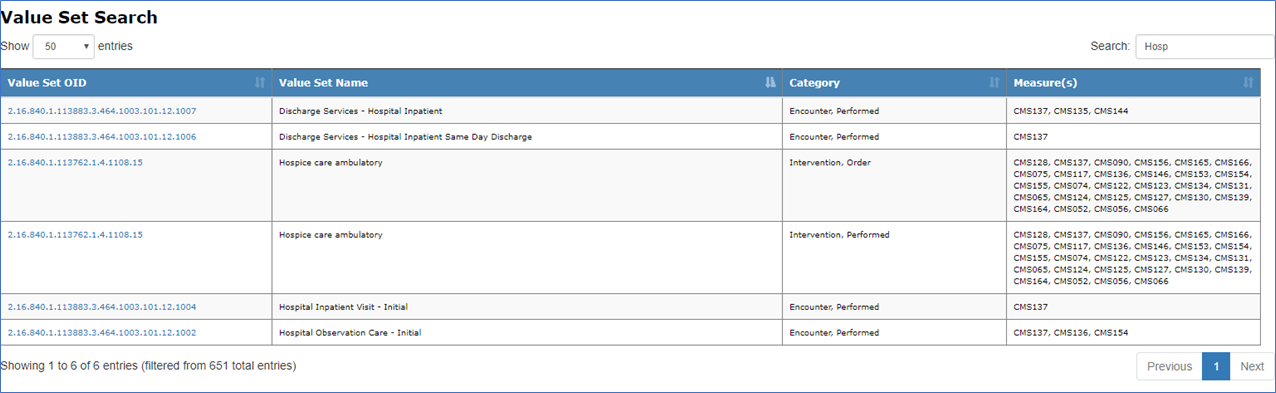
- Created a new report called Value Set Search that allows users to access and search value set information.
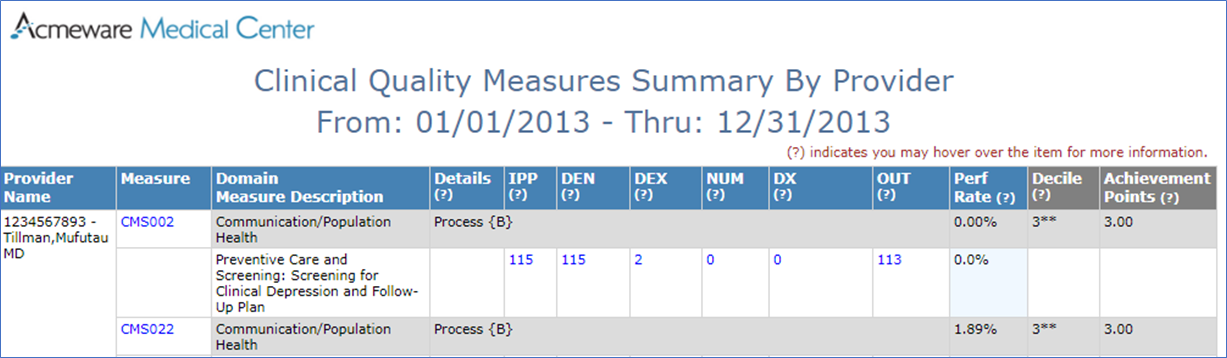
- Updated CQM report to include NPI with provider name.
- Updated Value Set Measure Summary to remove previous year comparison option.
Please review our help guides on Validation Reports and Mapping Reports. The help guides will highlight the tools OneView has available to assist in your measure validation process.
Clinical Quality Measures (CQM):
- Added 2 new measures:
- CMS347 - Statin Therapy for the Prevention and Treatment of Cardiovascular Disease
- CMS645 - Bone density evaluation for patients with prostate cancer and receiving androgen deprivation therapy
- Updated CQM benchmarks (deciles) for 2018 reporting period.
Fixes: (for all platforms unless specified)
Please Note: Customer Support Tickets referenced below may be Acmeware client specific and are not visible to all client on the Customer Support Portal.
Advancing Care Information (ACI) and Objective Measures (OM):
- ALL:
- Corrected issues with acute care only sites reporting ACI/OM measures.
- Identify provider by NPI rather than MEDITECH Provider ID.
- 6.15 - Reset invalid timestamps for BAR Transactions to midnight.
- Patient Specific Education (PSE) Measure:
- Correction for PSE issues resulting in low performance and numerator values.
- Corrected issues with PSE measures calculation for acute providers calculation where it was excluding all acute providers instead of including all acute providers.
- Health Information Exchange (HIE) Measure:
- Corrected issues with HIE measures calculation for acute providers calculation where it was excluding all acute providers instead of including all acute providers.
- Excluded disposition types from HIE using lookup table to allow for client customization without code changes. This change is part of HISP/HIE integration.
- Electronic Prescribing (EP) Measure:
- Updated EP measure to exclude prescriptions outside of the reporting period.
- Medication Reconciliation (MR):
- Corrected MR to include missing patients from the denominator. For both acute care and ambulatory providers, the performance rate would be inaccurate, as we were excluding patients that were in denominator but did not make the numerator for the denominator counts. For ambulatory providers only, performance rate would be accurate.
- Computerized Provider Order Entry (CPOE) Measure:
- Updated CPOE measure to include missing Providers. Customer Support Ticket: #3813
Clinical Quality Measures (CQM):
- Identify provider by NPI rather than MEDITECH Provider ID.
- 6.15 - Reset invalid timestamps for BAR Transactions to midnight.

